Agentic automation for healthcare takes care of business so you can take care of patients
UiPath customers have used automation to take on over two billion hours of burnout-inducing administrative tasks so healthcare workers, clinicians, and patients can thrive.
UiPath Solutions for Healthcare
Prebuilt agentic solutions tackle the most burdensome processes in claims management, allowing your staff to focus on what matters most. By automating repetitive tasks and enhancing decision making, this solution creates measurable improvements in both operational efficiency and patient satisfaction.
Claims, processed. Care gaps, closed. Referrals, streamlined.
The administrative burden is high in healthcare. Support healthcare staff and patients with agentic automation trusted by healthcare organizations worldwide.
$382 billion
in savings for the healthcare industry by 2027 with intelligent automation
IDC, 2024
83%
of surveyed U.S. healthcare executives list boosting employee efficiency as a top priority
Accenture, 2024
95%
of healthcare leaders said GenAI will be transformative
Bessmer Venture Partners, 2025
Dive into healthcare and life sciences agentic automation solutions
75% of the top 100 health systems in the U.S. and 400+ healthcare clients use UiPath to automate across core business areas and use cases.
RELATED SOLUTION
Revenue cycle management
Automate the revenue cycle management lifecycle to protect margins, accelerate reimbursement, and reduce the cost to collect.
Related solution
Medical record summarization
Learn how you can use UiPath to deliver high-quality, compliant medical record summaries in minutes.
Related solution
Life sciences
From research and development to marketing and supply chain, learn how to use AI-powered automation in your organization.
Revenue cycle transformation at Mayo Clinic and UT Southwestern
Learn how leading health systems are reducing denials, accelerating cash flow, and freeing up staff time – shared live at Becker’s Healthcare Virtual RCM Summit.

Comprehensive agentic automation for healthcare
From initial appointment scheduling to prior authorization for treatment, agentic automation keeps processes running smoothly.
Reduce costs
Agentic automation reduces the cost of care across payer and provider functions.
Orchestrate workflows
Agentic automation intelligently allocates work, boosting efficiency and trust.
Improve experiences
Agentic automation cuts waiting times while taking the pressure off staff.
In a world of point solutions, the UiPath Platform™ does it all
The AI-powered support team that’s always on call
- Claims operations
- Care management
- Revenue cycle management
- Supply chain
Accurate, timely, low-cost claims processes
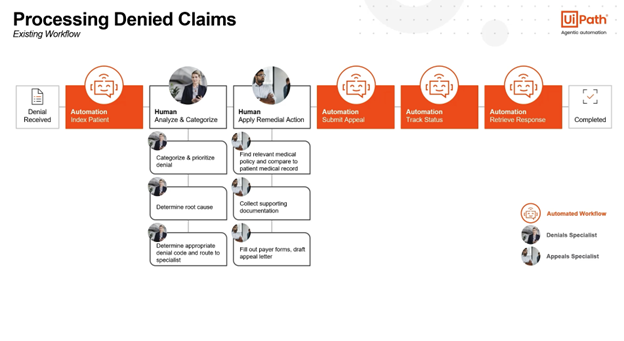
Streamline every part of the claims process to boost accuracy, speed up resolution, reduce costs, and stay compliant. Increase the volume of high dollar claims audits and reduce overpayments, automate up to 100% of the pending claims resolution process, and reduce overall turnaround time for appeals and grievances.

Reach more members at scale
Automate core processes in the care management value chain, from prior authorization to closing gaps in care. Drive faster turnaround time and scale member outreach using future-proof technology.

Maximize reimbursement and minimize cost to collect
From patient access through denials resolution, streamline operational processes across the entire revenue cycle lifecycle to accelerate cash flow and protect margins.

Cut costs, optimize inventory, and reduce administrative time and errors
Our supply chain agentic solutions streamline operations by automating invoice matching and validation, optimizing inventory levels with real-time tracking and predictive analytics, and ensuring data accuracy through automated master data governance. By reducing manual workloads, minimizing errors, and enhancing operational efficiency, organizations can achieve cost savings, improve supply chain resilience, and focus on delivering exceptional outcomes.

More to explore in healthcare
Cut costs and accelerate claims processing with agentic automation
Manual processes and outdated systems are slowing down your claims operations. The UiPath Platform for agentic automation is the key to reducing costs and speeding up claims resolution.
From gaps to gains: how automation transforms care gaps management
In healthcare, even small care gaps—missed screenings or overdue follow-ups—can lead to serious complications, poor patient outcomes, and lower compliance ratings. Learn how AI and automation streamline the process of closing gaps in care.
Fast-track provider credentialing: how automation reduces delays and boosts revenue
Delays in credentialing mean delayed revenue, limited patient access, and increased compliance risks. In this webinar, you’ll learn how AI and automation accelerates credentialing while improving data integrity and compliance.